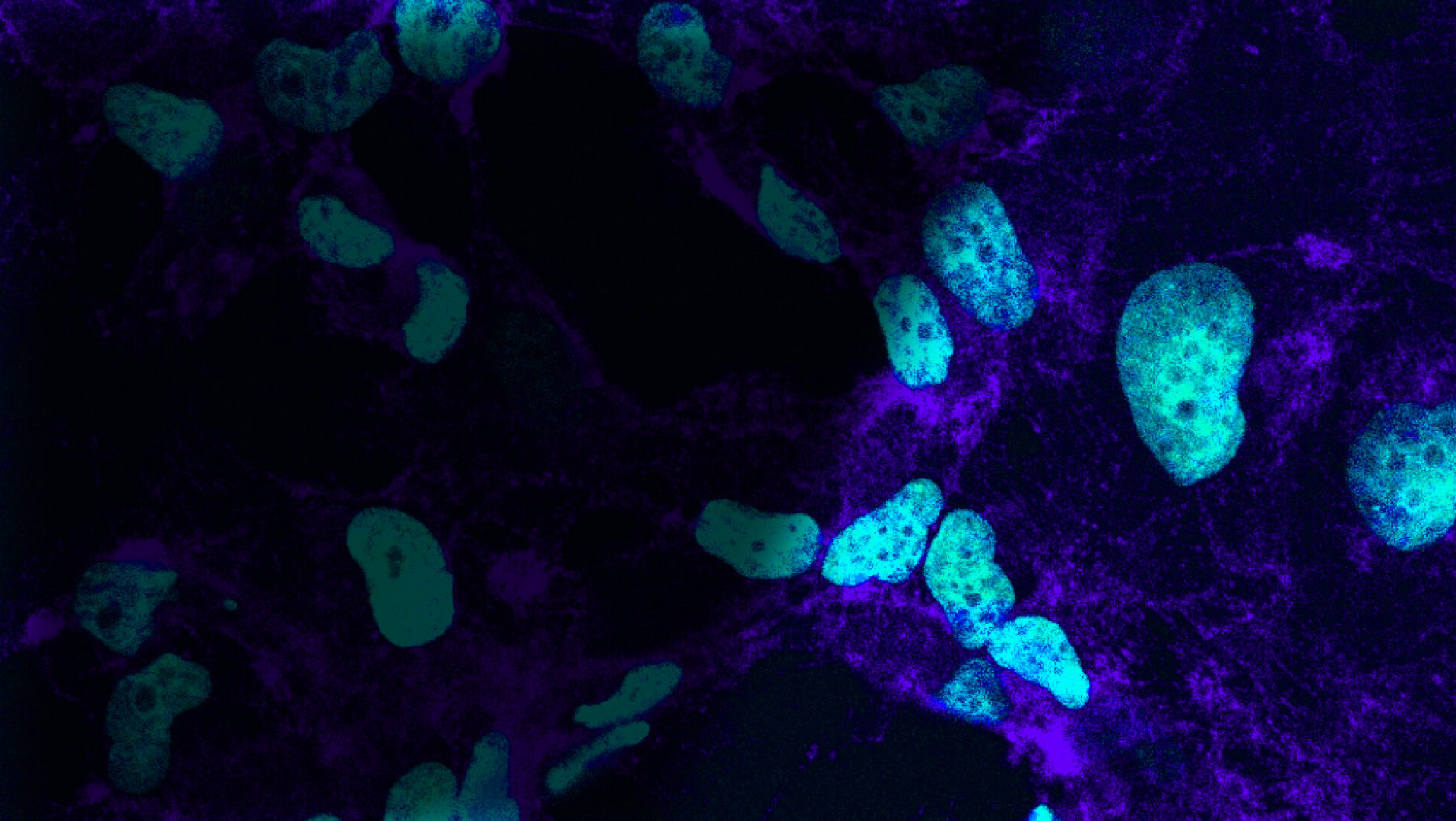
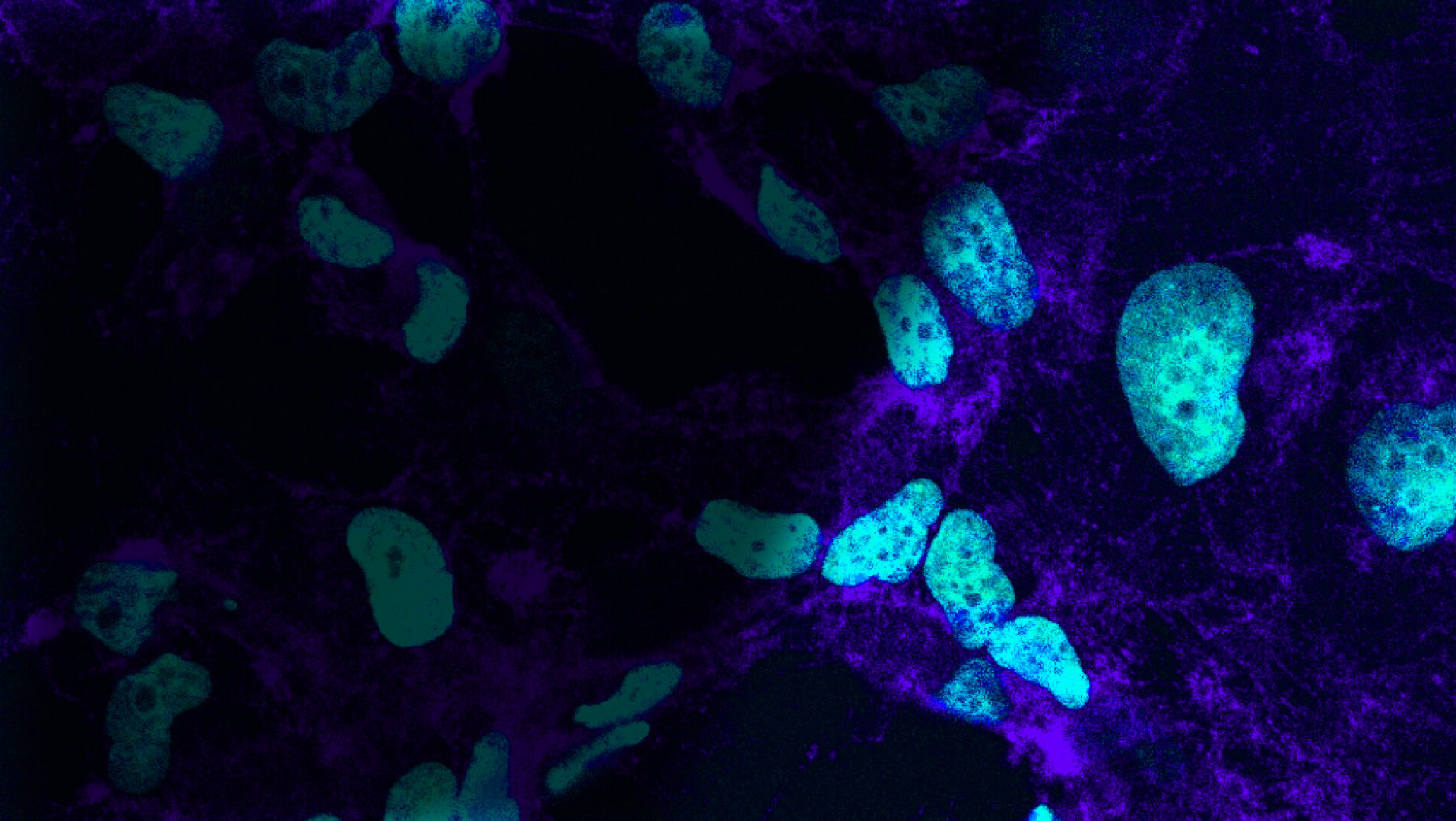
Unmasking cancer cell camouflage
with multifunctional fusion proteins
SITE IS CURRENTLY
BEING UPGRADED
For more information see
our investor presentation
Contact us at: [email protected]
BEING UPGRADED
For more information see
our investor presentation
Contact us at: [email protected]
Unmasking
cancer cell
camouflage
cancer cell
camouflage